TL;DR- A child medical consent form authorizes caregivers to make medical decisions for minors when parents or guardians cannot be present during treatment or emergencies
- Complete child identification, medical history including allergies, chronic conditions, and current medications must be included to enable proper emergency treatment
- Caregiver details, parent or guardian information, emergency contacts, and insurance information ensure healthcare providers can communicate with authorized parties
- Specific treatment authorization language clarifies which medical procedures caregivers can consent to, preventing confusion during urgent medical situations
- Proper signatures from parents or guardians with dates create legally binding documentation that hospitals and clinics require for lawful medical treatment
- Ziji Legal Forms provides comprehensive child medical consent form templates that ensure all critical information is included to protect child safety and legal compliance
Introduction: Why Child Medical Consent Forms Matter
Parents and guardians cannot always be physically present when children need medical care. Whether traveling on vacation, attending school camps, staying with relatives, or participating in after-school activities, situations regularly arise where trusted caregivers must make medical decisions on behalf of children.
A child medical consent form is a legally binding document that grants temporary medical decision-making authority to designated caregivers when parents cannot be present. This form ensures children receive necessary medical treatment promptly without dangerous delays caused by inability to reach parents or legal guardians for treatment approval.
Understanding what information must be included and avoiding common mistakes protects your child's health while establishing legal clarity for healthcare providers and caregivers.
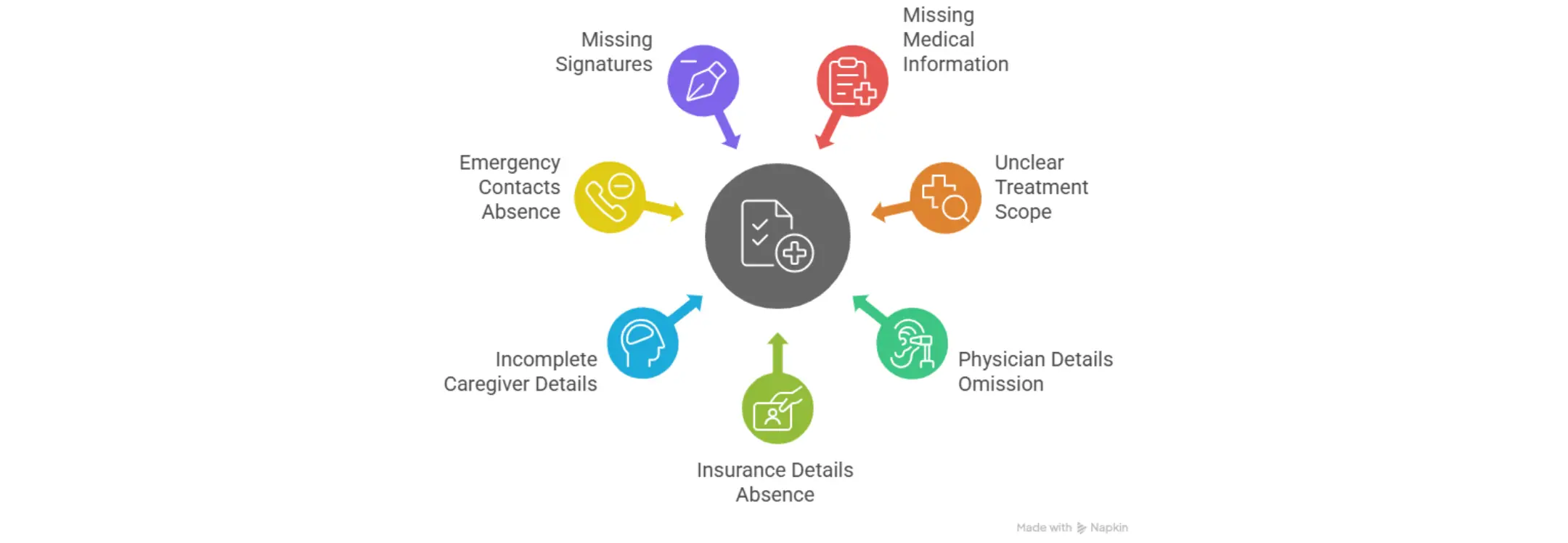
Mistake 1: Missing the Child's Full Medical Information
The Risk of Incomplete Medical History
Omitting essential medical information creates serious risks during emergencies when healthcare providers must make rapid decisions about treatment. If caregivers or healthcare providers lack knowledge about allergies, chronic conditions, current medications, or previous adverse reactions, treatment decisions could harm rather than help the child.
Medication allergies represent particularly critical information. A provider unaware of a child's penicillin allergy might prescribe an antibiotic triggering life-threatening allergic reactions. Incomplete medical history transforms a treatable medical problem into a dangerous emergency.
Essential Medical Details to Include
Complete child medical information should specify all known allergies including drug allergies, food allergies, and environmental allergies. Include chronic medical conditions like asthma, diabetes, epilepsy, or heart conditions that affect treatment decisions. List all current medications with dosages to prevent dangerous drug interactions or accidental overdoses. Note any previous surgeries or hospitalizations that might affect current treatment recommendations.
Emergency Response Impact
Healthcare providers making treatment decisions rely on accurate, complete medical histories. Emergency room physicians must make split-second decisions about which medications are safe and which treatments are appropriate. Missing information creates dangerous uncertainty that can delay treatment or result in contraindicated medical care.
Mistake 2: Unclear Scope of Medical Treatment Authorization
General Versus Specific Treatment Permissions
Vague or overly broad treatment authorizations create confusion about exactly what medical decisions caregivers can make without contacting parents. Healthcare providers need clear guidance about which treatments caregivers can approve immediately versus which treatments require parental contact.
Some parents want caregivers to authorize emergency care, surgery, and hospital admission when medical necessity exists. Others may want to limit caregiver authority to routine care only, requiring parental contact for any significant procedures. These preferences must be explicitly documented.
Why Hospitals Require Clarity
Hospital admissions, surgeries, anesthesia, blood transfusions, and other significant medical procedures typically require informed consent. Healthcare providers cannot proceed with procedures outside the authorization scope, potentially delaying necessary treatment. Clear authorization prevents treatment delays while respecting parental control over medical decision-making.
Scope of Authorization Language
Effective forms specify that caregivers can authorize emergency medical care deemed necessary by physicians to preserve the child's life or health. Some forms authorize routine medical care including office visits, vaccinations, medications, and diagnostic testing. Others specify treatments caregivers cannot authorize, requiring direct parental contact for those decisions.
Mistake 3: Not Listing the Child's Primary Physician
Importance of Doctor Contact Information
Missing primary physician information prevents hospitals and emergency departments from contacting the child's regular healthcare provider for relevant medical history, ongoing treatment information, and medication management guidance. Emergency physicians benefit enormously from consultation with a child's regular doctor who understands the child's complete medical history and baseline health status.
The primary physician provides continuity of care by understanding treatment history, successful treatments, ineffective approaches, and longstanding medical relationships that emergency providers lack. Including this contact information enables comprehensive, coordinated emergency care.
Emergency Verification Support
Healthcare providers can verify medical history information, confirm medication allergies, and ask about previous adverse reactions that might not be documented in emergency records. Primary physicians often have information about subtle medical issues, medication sensitivities, or family medical history that emergency physicians need for appropriate treatment decisions.
Mistake 4: Not Adding Insurance Details
Complete Insurance Information Requirements
Missing or incomplete insurance information creates billing confusion and potential payment denials when children receive emergency medical care. Healthcare providers must verify insurance coverage before treatment to secure payment authorization and understand coverage limits that might affect treatment recommendations.
Include the insurance provider name, complete policy number, group number if applicable, and emergency customer service hotline for immediate coverage verification. This information enables rapid payment authorization without delaying necessary medical care.
Emergency Admission Complications
Incomplete insurance information can trigger treatment denials if providers cannot verify coverage before proceeding. Some emergency procedures cannot wait for insurance verification, but missing information creates billing complications afterward. Complete insurance details enable rapid verification protecting payment authorization and preventing billing disputes.
Mistake 5: Incomplete Caregiver Details
Verification Requirements at Hospitals
Insufficient caregiver identification information prevents hospitals from verifying that the person presenting the consent form actually has authority to make medical decisions for the child. Healthcare providers must confirm that the person claiming to be an authorized caregiver has legitimate authority before following their medical instructions.
Hospitals typically verify caregiver identity through government-issued identification and may contact parents to confirm that the person presenting consent forms is truly authorized to make medical decisions.
Essential Caregiver Information
Complete caregiver information includes full legal name, relationship to the child, complete mailing address, phone number, and alternative contact information. This enables hospitals to verify caregiver identity against the consent form and contact them with treatment updates or questions.
Mistake 6: Not Including Emergency Contacts
Secondary Contact Necessity
Missing secondary emergency contacts prevents healthcare providers from reaching responsible adults if the primary caregiver becomes unavailable or if decisions arise beyond the caregiver's authority. Multiple emergency contacts ensure that someone can always be reached to provide additional authorization or guidance.
Secondary contacts should include another family member, close friend, or relative who understands the child's medical situation and can make decisions in emergencies if the primary caregiver cannot be reached.
Contact Information Requirements
Emergency contact details should include full names, relationship to the child, phone numbers including cell and home phone, and mailing addresses. Multiple phone numbers increase the likelihood of reaching someone rapidly in genuine emergencies when minutes matter.
Mistake 7: Missing Signatures or Witness Information
Signature Placement and Requirements
Unsigned or partially signed consent forms lack legal validity because they do not demonstrate that parents or guardians actually authorized the medical decisions the form describes. Healthcare providers cannot proceed based on unsigned documents because no proof exists that legitimate authority granted the caregiver medical decision-making power.
Both parent or guardian signatures with printed names, dates, and times create legal documentation proving that authorized individuals agreed to the medical decisions the form permits.
Witness Considerations
While not always required, having a witness present during signing provides additional verification that the parent or guardian voluntarily signed the consent form without coercion. Witnesses should be neutral third parties who are not family members and can verify that the signing occurred without pressure.
Optional Notarization
Some situations benefit from notarization to provide additional legal formality and verification that the parent or guardian identity was verified by a public official. Notarized forms carry additional legal weight in some jurisdictions and situations, though most consent forms do not require notarization.
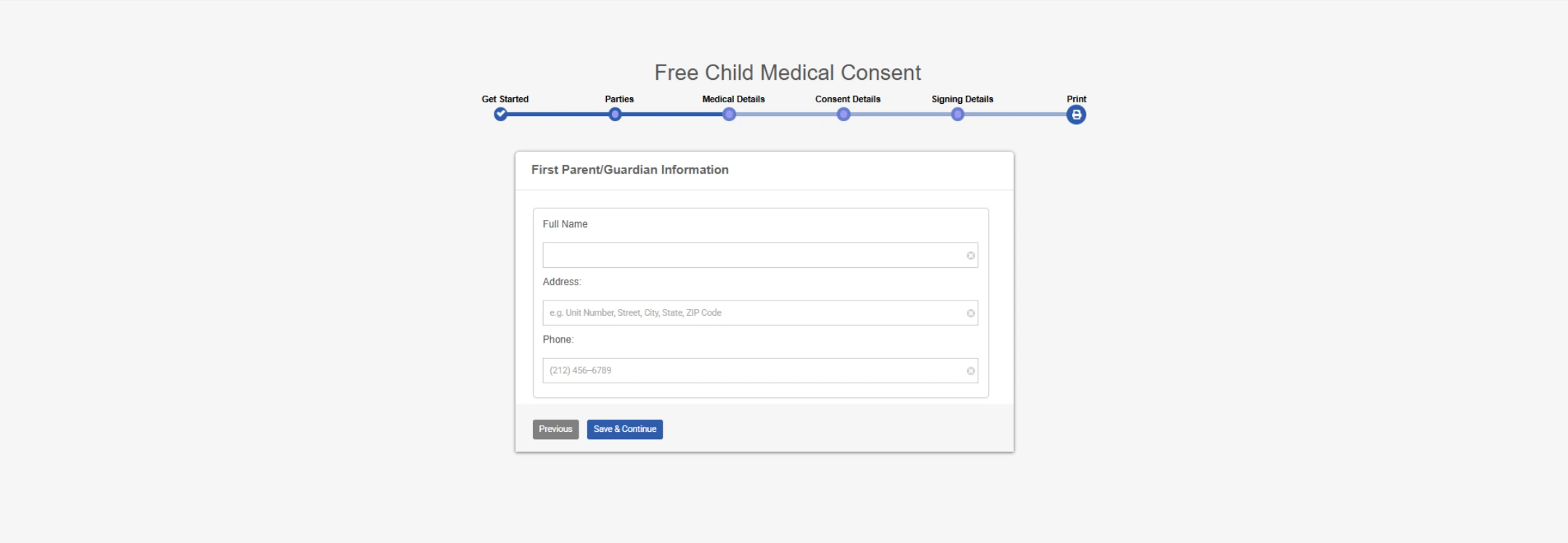
How to Create a Child Medical Consent Form Using Ziji Legal Forms
Using Ziji Legal Forms reduces common mistakes by guiding you through every required field and ensuring all medical, legal, and contact details are complete and accurate.
1. Choose template
Access Ziji Legal Forms' Family and Personal section and select the Child Medical Consent Form Template designed to include all essential child medical information and legal requirements.
2. Add Party Details
Enter the child's full name, date of birth, address, and parent or guardian names with contact information to establish clear identification and communication channels.
3. Add Medical Details
Include complete medical information including all allergies, chronic medical conditions, current medications with dosages, vaccination history, preferred healthcare providers, and any other relevant medical history.
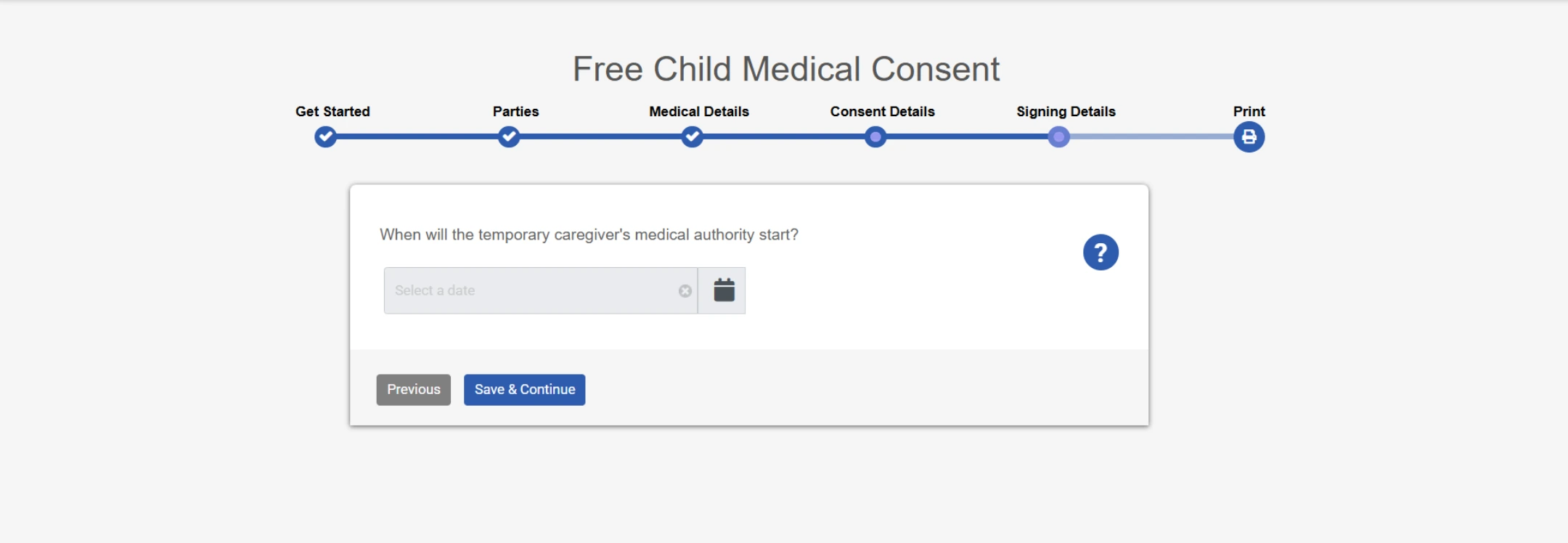
4. Add Consent and Signing Details.
Specify the exact medical treatments and procedures caregivers can authorize, emergency contact information, insurance details, and dates when the authorization becomes effective and expires.
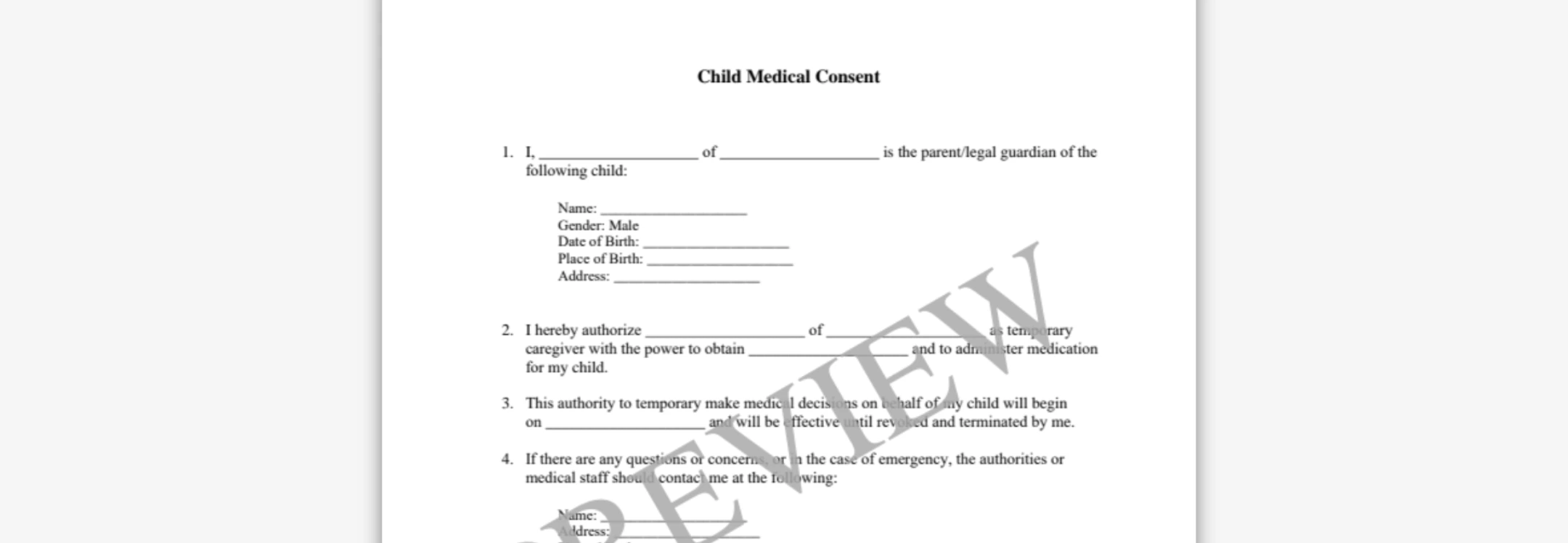
5. Preview and print.
Review the completed form thoroughly to ensure all information is accurate and complete, then download in PDF or Word format for printing and signature by parents or guardians.
Benefits of Using Ziji Legal Forms to Create Your Child Medical Consent Form
- Ziji Legal Forms provides step-by-step guidance to complete every required field, reducing omissions and errors.
- Templates reflect legal best practices, so your form complies with medical and privacy laws at the federal level.
- All critical medical, contact, and authorization details are prompted, helping avoid delays in emergency care.
- Customization options let parents update forms easily for new caregivers or medical situations as needed.
- Instant download and print features mean families never have to wait or worry about last-minute medical consent.
Conclusion: Protect Your Child with Complete Medical Authorization
Child medical consent forms ensure your child receives necessary medical care promptly while maintaining your control over medical decision-making through clear authorization guidelines. Using Ziji Legal Forms' comprehensive templates eliminates the most common documentation errors that compromise child safety or create legal confusion for healthcare providers.
Child Medical Consent FAQs
What is a child medical consent also known as?
A child medical consent is also known as the following: child medical release form, consent to treat minor children, medical release form for minor, or treatment authorization form for minor.
What is child medical consent?
A child medical consent form is a document that parents/legal guardians can use to authorize another adult to make medical decisions for a minor child. Accidents and emergencies involving children are very common so it is prudent to plan for them by having a medical consent form for your child. A child medical consent form can prevent delays in medical treatments in cases of emergency when doctors and other healthcare providers cannot reach you, for example, your child having allergic reaction while staying at summer camp, or suffering from injuries at a sporting tournament.
When should you use a child medical consent?
If your child will be away from the parents/guardians for extended period of time, you should use a child medical consent to authorize another supervising adult to grant medical consent on your behalf. For example, you may be away for an extended period for work or travel or when the child will be traveling or staying with a supervising adult in your absence.
Who can be the temporary guardian that makes medical decision for your child?
Any adult who is at least 18 years old can be the temporary guardian. The individual you pick should be someone responsible, and respects your beliefs and wishes relating to medical treatments. For example, a temporary guardian that will be making medical decisions for your child could be:
- A grandparent
- An aunt or uncle
- A close family friend
- A teacher
- A babysitter
What should you include in the child medical consent?
The child medical consent should cover the following:
- The parent’s full name and contact information including full address and phone number.
- The child’s full name and health information including the child’s allergies, special needs, medication and illness history, and health insurance if applicable.
- The temporary guardian’s full name and phone number.
- The specific medical treatments the temporary guardian will be allowed to grant consent for your child. For example, blood transfusion or vaccine use.
- The full name and contact information of your child’s doctor, especially if the doctor is a specialist treating your child’s special medical conditions.
- A start date and end date to limit the duration of the power that’s granted for the temporary guardian. If you do not know how long you will be away from your child, you may leave out the end date then the child medical consent will be valid until you revoke it at a future date.
When should you use a child medical consent and a child travel consent?
A child travel consent only grants the permission to your child to travel alone or with a designated adult without the parents or legal guardians. A child medical consent authorizes an adult that is not the parent or legal guardian to make medical decisions for your child. They are often used together but they are different consent forms and cannot be substituted with each other. It would be prudent to have both documents completed and notarized before your child travels in your absence.
Can I revoke a child medical consent after it has been given?
Yes. You can cancel or revoke the consent at any time by providing written notice to the temporary guardian and, if possible, to any healthcare providers who may have received a copy of the consent form. It is important to keep a record of the revocation to avoid confusion in an emergency situation.
Does a child medical consent need to be notarized?
While notarization is not always legally required, it is highly recommended. A notarized form helps confirm the authenticity of the signature and can make it more readily accepted by healthcare providers, schools, and other institutions.
How long is a child medical consent valid?
The validity of the consent depends on the dates specified in the form. You can set a specific start and end date, or allow it to remain in effect until you revoke it. It’s best to choose a timeframe that matches your child’s planned activities or travel schedule.
Can more than one temporary guardian be named in the form?
Yes. You can name multiple adults who are authorized to make medical decisions for your child. This is often helpful if the child will be in the care of different people at different times, but be sure to clearly outline whether each guardian has equal authority or if certain decisions require a specific person.
Is a child medical consent valid in another state or country?
Generally, a properly executed child medical consent will be recognized in other states, but the rules can vary. If your child will be traveling internationally, it is best to check the destination country’s requirements, as some may require additional documentation or translations.
What jurisdictions can use our child medical consent form?
You can use our template to create a legal and valid child medical consent form for the following jurisdictions:
|
Alabama
Alaska
Arizona
Arkansas
California
Colorado
Connecticut
Delaware
District of Columbia
Florida
Georgia
Hawaii
Idaho
Illinois
Indiana
Iowa
Kansas
Kentucky
Louisiana
Maine
Maryland
Massachusetts
Michigan
Minnesota
Mississippi
Missouri
Montana
Nebraska
Nevada
New Hampshire
New Jersey
New Mexico
New York
North Carolina
North Dakota
Ohio
Oklahoma
Oregon
Pennsylvania
Rhode Island
South Carolina
South Dakota
Tennessee
Texas
Utah
Vermont
Virginia
Washington
West Virginia
Wisconsin
Wyoming |
AL
AK
AZ
AR
CA
CO
CT
DE
DC
FL
GA
HI
ID
IL
IN
IA
KS
KY
LA
ME
MD
MA
MI
MN
MS
MO
MT
NE
NV
NH
NJ
NM
NY
NC
ND
OH
OK
OR
PA
RI
SC
SD
TN
TX
UT
VT
VA
WA
WV
WI
WY |